Understanding AI’s Role in Healthcare: A Framework for Boards and CEOs
Aligning Board and Leadership Expectations
Healthcare providers face intense pressure to improve clinical outcomes, manage costs, and enhance patient and employee experiences. Increasingly, boards and executive teams are exploring artificial intelligence (AI) as a strategic lever to address these multifaceted challenges. Drawing on lessons from its engagements with diverse healthcare clients—from specialty practices to large integrated health systems—Avancer, a strategic advisory firm, helps leaders adapt their governance and leadership strategies to leverage AI’s potential effectively. This guidance encompasses prioritizing AI opportunities, framing associated risks, and pursuing key objectives such as cost containment, quality improvements, and developing new and expanded revenue streams. Given these pressures and possibilities, a clear, objective framework is essential for evaluating how AI can best integrate into an organization’s strategy, streamline operations, and strengthen its market position.
Translating AI’s promise into tangible results is not straightforward. While almost all healthcare providers deploy regulatory-approved AI solutions, they must still ensure safe and effective workflow use, maintain compliance with data privacy laws, provide clinical training and monitoring, offer technical support, manage ongoing maintenance and planned obsolescence (replacement), and address interoperability challenges. Success also hinges on organizational readiness, precise strategic alignment, and honest assessments of AI’s capabilities and what will be unknown limitations. By adopting a fact-based, informed approach—grounded in a real-world framework—boards and leadership can mitigate risks and ensure that AI investments deliver meaningful value over their lives.
Understanding AI in Healthcare
Even when licensing pre-built AI solutions, healthcare providers must understand the underlying data-driven techniques these tools use for prediction, classification, or insight generation. This understanding is crucial for safe use, effective deployment, long-term interoperability, and monitoring of the AI solution’s life. Each model type has distinct data requirements, validation needs, interpretability levels, maintainability (e.g., new ‘learnings’), and regulatory dependencies. Aligning the appropriate model with organizational objectives—such as enhancing revenue, improving clinical outcomes, or streamlining operations—maximizes AI's potential:
Supervised Learning Models: This method uses labeled data (where the desired output is already known) to train a model to predict or classify outcomes. The model learns the relationship between input features and the correct output. Examples include:
Detecting abnormalities in medical images (e.g., identifying cancerous tumors in X-rays or CT scans): The images are labeled by radiologists as "benign" or "malignant," and the model learns to distinguish between them.
Patient data (e.g., demographics, diagnoses, prior admissions, etc.) is used to predict the likelihood of a patient being readmitted within a specific timeframe.
Predicting patient risk scores for specific conditions (e.g., sepsis, heart failure) based on patient vitals, lab results, and medical history, the model predicts the likelihood of developing a specific condition.
Unsupervised Learning Models: This method works with unlabeled data, identifying patterns, structures, and groupings without prior knowledge of the desired output. Examples include:
Grouping patient populations based on similar characteristics (e.g., disease progression, treatment response) to identify subtypes of diseases or personalize treatment strategies.
Uncovering cost drivers in service lines by analyzing claims data to identify factors contributing to high costs, such as specific procedures, patient demographics, or geographic locations.
Identifying unusual patterns in patient data, such as unexpected spikes in hospital admissions or adverse drug events.
Natural Language Processing (NLP) and Large Language Models (LLMs): This model interprets text-based information (e.g., clinical notes, research literature, claims) to streamline documentation, highlight relevant guidelines, and reduce administrative burden. NLP is a field focused on enabling systems to understand and process human language. LLMs are a powerful form of NLP model capable of generating and understanding text at scale. Examples include:
Extracting key information from clinical notes by automatically identifying diagnoses, symptoms, medications, and other relevant details.
Providing concise summaries of scientific literature to help clinicians stay up-to-date.
Streamlining the process of obtaining insurance approval for procedures or medications.
Providing automated responses to patient inquiries and scheduling appointments. These tools can also optimize coding and billing.
Emerging AI Models: Advanced approaches like federated learning (enabling privacy-preserving model training on decentralized data), semi-supervised learning, advanced LLM-based conversational agents, reinforcement learning (potential for personalized treatment plans), and transfer learning offer future potential. However, broader adoption is likely further out due to evolving regulatory frameworks, the need for more robust clinical effectiveness evidence, and organizational readiness.
Prioritizing AI Opportunities
Healthcare providers operate within a complex landscape of reimbursement models, each with distinct incentives and priorities. These models—from traditional fee-for-service (FFS) to value-based care (VBC) and various alternative payment models—significantly influence strategic decision-making, including investments in new technologies like AI. Therefore, a crucial step in effectively leveraging AI is aligning its application with the specific financial and clinical goals dictated by the prevailing reimbursement structures and total cost of care. This lens by leadership ensures that AI investments directly support organizational success within the current and anticipated payment environment:
Fee-for-Service (FFS): This model reimburses providers for each service rendered. This incentivizes volume with quality of care. AI applications in this model focus on optimizing operational efficiency and maximizing revenue capture through accurate coding and billing. Examples of AI's application:
Improving coding accuracy: NLP can analyze clinical documentation to ensure accurate coding and maximize reimbursements.
Reducing claim denials: AI can identify potential coding errors before claims are submitted, reducing the likelihood of denials.
Optimizing scheduling and resource allocation: AI can predict patient demand and optimize staffing and resource allocation to improve efficiency.
Value-Based Care (VBC) / Prevention-Oriented Models: These models tie reimbursement to patient outcomes and quality of care. AI applications in this model focus on improving patient outcomes, reducing costs through preventive care and care coordination, and improving quality metrics. Examples of AI's application:
Identifying high-risk patients for targeted interventions: Predictive models can identify patients at high risk of hospitalization or other adverse events, allowing for proactive interventions.
Personalizing treatment plans: AI can analyze patient data to develop personalized treatment plans that are more effective and efficient.
Improving care coordination: AI can facilitate communication and information sharing between different care providers, improving care coordination and reducing fragmentation.
Population health management: AI can analyze population-level data to identify trends and develop targeted interventions to improve the health of specific populations.
While fee-for-service (FFS) and value-based care (VBC) represent two dominant healthcare provider models, numerous other reimbursement models exist, including bundled payments, shared savings programs, capitation, and episode-based payments, these other healthcare models often blend elements of FFS and VBC or introduce unique incentives related to specific episodes of care, populations, or quality metrics. The principles of aligning AI applications with reimbursement incentives remain relevant across all models, even though the particular applications and their prioritization may vary.
AI Model Applications
Healthcare providers must navigate a complex regulatory landscape concerning AI adoption, adhering to standards and guidance from various agencies. These include governmental bodies like the FDA, ONC, NIST, and HHS, which focus on safety, interoperability, and risk management; professional organizations such as the AMA, AHIMA, and RSNA, which emphasize ethical considerations and best practices; and international organizations like the WHO and ISO, which promote global standards. This diverse regulatory environment necessitates ongoing monitoring and compliance efforts to ensure responsible and effective AI implementation in healthcare.
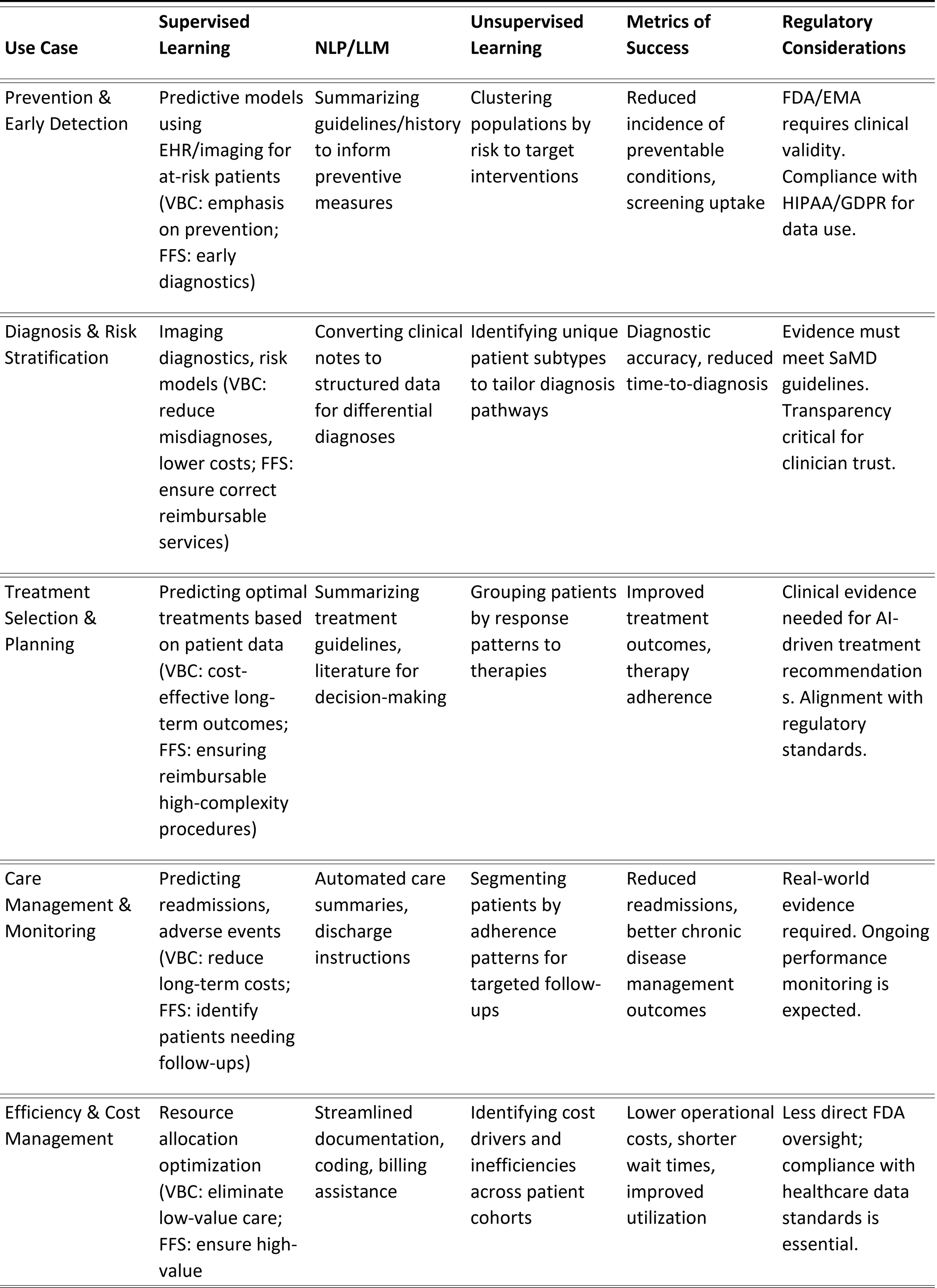
The table below offers a framework of how AI learning models can address key healthcare challenges in a patient’s continuity of care, from prevention and early detection to care management and cost containment. In addition, it highlights potential success metrics and notes regulatory considerations:
Governance and Leadership Considerations
Incorporating AI into healthcare strategies requires more than technical expertise. Boards and leadership must adapt governance practices and competencies to guide AI investments effectively. This shift involves acknowledging that AI can introduce new revenue streams, alter existing ones, reshape workforce roles, and raise unique ethical and compliance challenges. Leaders must establish robust oversight structures, ensure responsible data use, and foster trust in AI-driven insights across the organization:
Strategic Alignment: Ensure AI initiatives are closely linked to the organization’s mission, incentive structures, and strategic goals. Investments should deliver tangible financial and clinical returns that reinforce core priorities.
Governance Structures and Oversight: Consider establishing dedicated AI committees or augmenting board expertise with directors possessing backgrounds in data science, digital health, or relevant regulations. This enhances the board’s capacity to scrutinize AI projects, assess their impact on care delivery, patient safety, and organizational performance, and ensure alignment with evolving regulatory requirements.
Long-Term Investment Perspective: AI maturity is a journey, not a destination. Boards and leadership must adopt a long-term view, prioritizing foundational investments in data quality, interoperability, and scalable platforms. This gradual capability-building ensures organizational adaptability to evolving technologies and regulatory requirements.
Data Compliance Competencies: Strengthen internal expertise in data governance, privacy, and security, including familiarity with relevant regulations (e.g., HIPAA, GDPR). Robust data standards and practices are essential for safe, compliant AI deployment, regulatory confidence, and public trust.
Risk Management and Ethical Considerations: Proactively identify potential risks, such as biased algorithms, privacy violations, patient safety issues, and algorithmic opacity (lack of explainability). Incorporate risk mitigation strategies, ethical frameworks, and clear accountability measures to ensure that AI supports fair, responsible, transparent, and patient-centered care.
Cultural Adaptation and Workforce Readiness: Train clinicians, managers, and frontline staff to understand, trust, and effectively use AI tools. Consider adjusting organizational structures, such as appointing a Chief AI Officer or embedding AI specialists within clinical teams. Encourage ongoing feedback, transparent communication, and change management strategies to build trust, promote adoption, and ensure that AI augments rather than replaces human judgment.
Preparing for Sustainable AI-Driven Growth
AI offers healthcare providers pathways to enhance revenue streams, improve patient outcomes, increase operational efficiency, and bolster both employee and patient satisfaction. Realizing these benefits, however, demands a deliberate and well-structured approach. Boards and leadership must understand AI’s learning models, strategically align opportunities with existing and emerging incentive structures, deploy solutions thoughtfully across the care continuum, and adapt governance and leadership practices to ensure responsible, ethical, and effective implementation.
Healthcare leaders can set the stage for sustainable, AI-driven growth by adopting a measured, evidence-based, and iterative approach. This approach leverages current opportunities and equips organizations to navigate evolving regulations, shifting payment models, and changing patient expectations in a dynamic healthcare landscape. Preparing positions healthcare providers to remain resilient, innovative, and responsive in an increasingly data-driven and technologically advanced industry.